Study type |
Phase I/II Interventional Multi-site |
| Location | UK |
| Therapeutic area | Oncology, Amyloidosis |
| Product | 90Y-anti-CD66 radiolabelled antibody |
| Sponsor | University Hospital Southampton NHS Foundation Trust |
Home » News and Events » Case Study » How PHARMExcel collaborated with ECMC to deliver a new revolutionary radiation therapy

Study type |
Phase I/II Interventional Multi-site |
| Location | UK |
| Therapeutic area | Oncology, Amyloidosis |
| Product | 90Y-anti-CD66 radiolabelled antibody |
| Sponsor | University Hospital Southampton NHS Foundation Trust |
"I have found the PHARMExcel team to be efficient, highly professional while being accommodating and very supportive. They are very interactive and excellent in communicating with clinical teams. They have a thorough understanding of the regulatory requirements for managing GCP compliant clinical trials. I have no hesitation in recommending them as a CRO. "
Dr Kim Orchard, Southampton ECMC
 Working in partnership with the Experimental Cancer Medicine Centre (ECMC) Network, PHARMExcel lead the phase I clinical trial TRALA (Targeted Radiotherapy for AL-Amyloidosis), researching a new transplant pre-conditioning technique developed by the Targeted Radiotherapy Group at Southampton ECMC, that may result in an improvement in the response rate post-transplant for S-ALA patients.
Working in partnership with the Experimental Cancer Medicine Centre (ECMC) Network, PHARMExcel lead the phase I clinical trial TRALA (Targeted Radiotherapy for AL-Amyloidosis), researching a new transplant pre-conditioning technique developed by the Targeted Radiotherapy Group at Southampton ECMC, that may result in an improvement in the response rate post-transplant for S-ALA patients.
This complex treatment allows very precise delivery of high radiation doses to the site of disease, in this case the clonal plasma cells, and avoids irradiating healthy organs in compromised individuals.
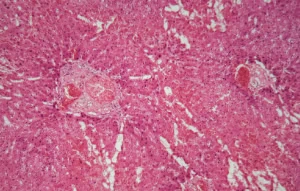
S-AL-amyloidosis is a serious haematological condition related to multiple myeloma and is characterised by the deposition of AL-amyloid protein fibrils in various organs such as the heart, liver, spleen, and kidneys. The protein is produced by clonal plasma cells present in bone marrow.
Most patients with S-ALA respond to similar treatments used to treat myeloma including high dose chemotherapy and autologous stem cell transplantation which can result in control of their disease and improvement in survival.
AL-A patients, however, are more difficult to treat as they often have additional medical problems such as impaired kidney and cardiac function which can result in significant toxicities associated with high dose chemotherapy. Even with careful patient selection and screening, the morbidity and mortality associated with autologous stem cell transplantation is much higher than for patients with myeloma.
 The Targeted Radiotherapy Group at Southampton ECMC developed a technique of preparing patients for transplantation using a radio-labelled monoclonal antibody that targets the bone marrow.
The Targeted Radiotherapy Group at Southampton ECMC developed a technique of preparing patients for transplantation using a radio-labelled monoclonal antibody that targets the bone marrow.
This complex treatment allows very precise delivery of high radiation doses to the site of disease, in this case the clonal plasma cells, and avoids irradiating healthy organs in compromised individuals.
The group at Southampton has previously shown that very high doses of radiation can be safely delivered to the bone marrow with minimal radiation to other organs. In theory, if radiation could be directed specifically to sites of disease in patients with Systemic-ALA then the benefits of radiation could be used avoiding the unwanted toxicity to normal organs.
The concept behind this study was to explore the use of a novel transplant conditioning agent (90Y-anti-CD66 radiolabelled antibody) in the context of a highly vulnerable patient group and to test the hypothesis that the radiolabelled antibody has disease reduction and efficacy.
If successful, this type of treatment could reduce transplant related morbidity and mortality associated with a standard transplant with high dose chemotherapy.
"The group has shown that very high doses of radiation can be safely delivered to the bone marrow with minimal radiation to other organs. If successful, the results of the study will be used to support a larger Phase II trial expanded to include more ECMCs in the UK."
Dr Kim Orchard, Southampton ECMC
 The lack of toxicity, particularly the complete absence of mucositis, but with disease responses would indicate that the 90Y-anti-CD66 could offer an effective treatment option for patients with S-ALA. Several new agents effective in myeloma have shown considerable activity in S-ALA including monoclonal antibodies such as Daratumumab. Although able to induce excellent responses, the majority of patients will relapse. While Autologous Stem Cell Transplant remains an option for S-ALA the use of targeted radiotherapy could play an important role in providing a method of consolidation or for treatment of relapsed/refractory disease with minimal toxicity.
The lack of toxicity, particularly the complete absence of mucositis, but with disease responses would indicate that the 90Y-anti-CD66 could offer an effective treatment option for patients with S-ALA. Several new agents effective in myeloma have shown considerable activity in S-ALA including monoclonal antibodies such as Daratumumab. Although able to induce excellent responses, the majority of patients will relapse. While Autologous Stem Cell Transplant remains an option for S-ALA the use of targeted radiotherapy could play an important role in providing a method of consolidation or for treatment of relapsed/refractory disease with minimal toxicity.
Future trials could explore the use of a standard dose of radiation to the bone marrow. In addition, DNA-damage repair inhibitors could be used to augment the beneficial effect of targeted radiation.
The TRALA study, funded by Leukaemia and Lymphoma Research (LLR) and the National Amyloidosis Centre (NAC) based at the Royal Free Hospital in London, demonstrates an excellent example of how PHARMExcel supports the innovation and development of new drugs through collaborative partnerships, such as with the ECMC network.
The Experimental Cancer Medicine Centres (ECMC) Network is uniquely placed to help industry develop the cancer drugs of the future, bringing together an unrivalled team of world-leading clinical experts, working collaboratively to deliver early phase clinical trials.
ECMC researchers are world-leading scientists and clinicians who drive the discovery, development and testing of new treatments to combat cancer. The funding supports over 200 staff involved in early phase trials and translational research.
PHARMExcel is an award-winning, full-service Contract Research Organisation (CRO) providing a flexible and innovative approach to clinical trial delivery. The company is recognised for its in-depth knowledge and experience of the clinical research environment, particularly in the UK, and has a network of regulatory and industry associates, allowing it to provide a global reach.
Media Contact
Katie Howe, Head of Marketing
E: [email protected]
T: +44 (0)20 3642 6654

ATMP Oncology Study: The first-in man trial for a Biotech’s novel therapy to prime the patient’s natural killer cells to attack their cancer
Read more

PHARMExcel named among the best CRO specialist providers
Read more

Case study: liver dialysis device, DIALIVE, proves safe and effective
Read more

Engaging patient and advocates in rare disease clinical trials
Read more
