In the medical research space, rare diseases occupy a unique and often overlooked corner. Defined by their low prevalence, these conditions collectively affect millions worldwide, presenting complex challenges for patients, families, and researchers alike. In the United Kingdom (UK), the pursuit of treatments and cures for rare diseases is steadily gaining momentum, fuelled by advancements in science, technology, and a growing recognition of the need for tailored interventions. Between 2016-2021 over 1.1 billion was invested by the UK Government and charities.
What is the definition of a rare disease
In the UK a rare disease is defined as one that affects less than 1 in 2,000 of the general population. According to a report published by The NIHR, there are between 5,000 and 8,000 known rare diseases. In the UK, a single rare disease may affect up to about 30,000 people, though the vast majority of rare diseases will affect far fewer than this.
Overcoming the hurdles of rare disease clinical trials
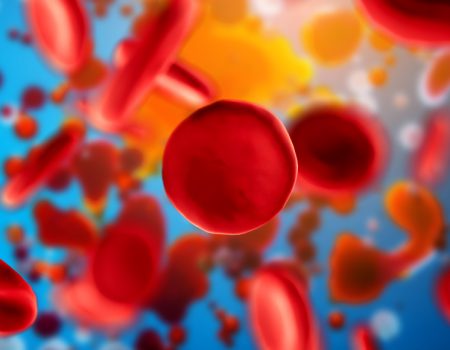
Over 1,800 drugs are undergoing clinical trials in various phases of development including preclinical and investigational drugs, with the majority targeted at oncology, followed by central nervous system, genetic, metabolic, haematological and respiratory disorders.
Clinical trials serve as the backbone of medical progress, offering a systematic pathway for testing new therapies and interventions. However, conducting trials in rare diseases presents a myriad of distinctive challenges, requiring careful consideration and specialised approaches.
Here are some key areas to consider when setting up a rare disease clinical trial:
- Site feasibility and patient recruitment
Unlike more prevalent conditions where patient recruitment may be relatively straightforward, recruiting participants for rare disease trials can be immensely challenging. Selecting a site that has experience in recruiting patients in the same therapeutic area as the study is paramount to meeting recruitment targets. A competent CRO will be able to recommend specialist sites and centres of excellence which they have existing relationships with. - Natural history studies and biomarker identification
Rare diseases often lack comprehensive natural history data, making it challenging to design robust clinical trials. Conducting natural history studies to clarify the disease progression and identify relevant biomarkers is crucial for informing trial design and outcome measures. These studies provide invaluable insights into disease heterogeneity, patient variability, and potential endpoints, ultimately enhancing the validity and interpretability of trial results. - Regulatory considerations and orphan drug designation
Regulatory pathways for rare disease therapies differ significantly from those for more common conditions. Obtaining orphan drug designation, which provides incentives and regulatory benefits for developing therapies targeting rare diseases, is often a pivotal step in the clinical trial process. Navigating the complex landscape of regulatory requirements, including orphan drug designation, orphan drug exclusivity, and adaptive trial designs, requires close collaboration between the Sponsor, the CRO and the regulatory agencies. - Collaborative networks and multi-centre trials
Recognizing the inherent limitations of single-centre studies in rare diseases, establishing collaborative networks and conducting multi-centre trials are essential for maximising patient recruitment, data collection, and generalisability of findings. Collaborative platforms such as the UK Rare Diseases Framework and European Reference Networks facilitate cross-institutional collaboration, enabling researchers to pool resources, share expertise, and collectively address the challenges of rare disease research. - Patient-centred outcomes and quality of life measures
Traditional clinical endpoints may not adequately capture the multifaceted impact of rare diseases on patients’ lives. Incorporating patient-centred outcomes and quality of life measures into trial protocols is essential for capturing the full spectrum of disease manifestations and treatment effects. Outcome measure selection should reflect relevance and significance for the patient; this may be diminished pain or itching, or a reduced requirement for daily care, and may include a relevant patient-related outcome measure. However, for rare diseases where the selection of measures or events expected to show only small changes or occur infrequently, run the risk of failure to demonstrate effect over the course of a trial.
Engaging patients, their families and carers in the selection of relevant outcome measures ensures that trial outcomes align closely with patients’ priorities and experiences.